Therapie des Endometrium-Karzinoms
Allgemeines
adenomatöse Hyperplasie
POLE-Mutation
pT1a pNx,o
Ladner - Ergebnisse
primär fortgeschrittenen oder rezidivierenden
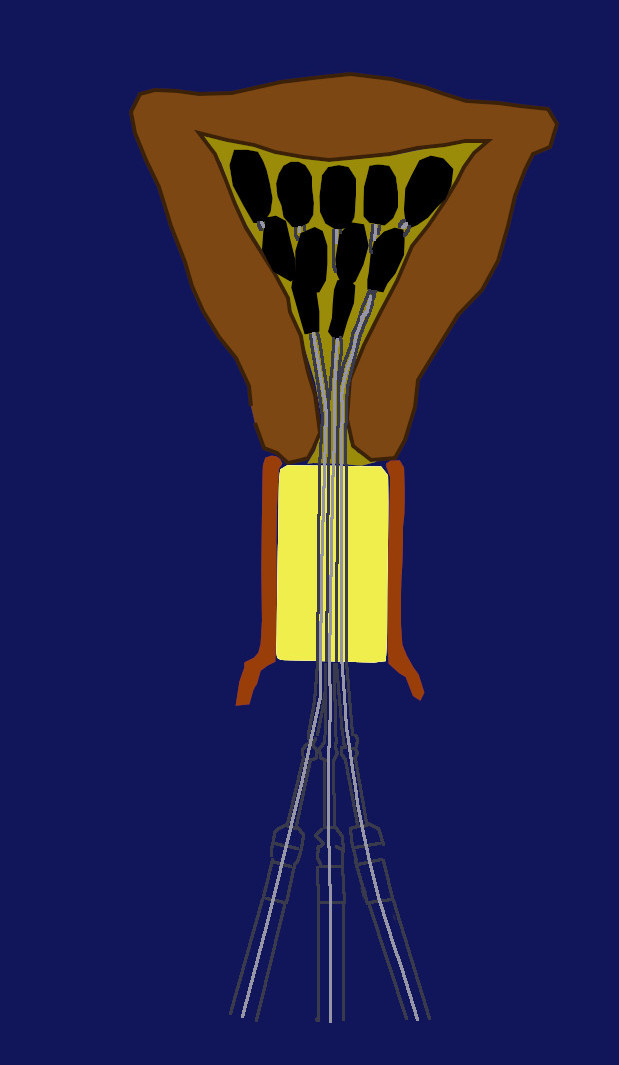
Operation (1)
Strahlentherapie
endokrine Therapie
Target - Therapie
Teil von
Quellen
Deutschen Gesellschaft für Gynäkologie und Geburtshilfe (DGGG).
01/2004
2.) Fleming GF, et al.:
Phase III trial of doxorubicin plus cisplatin with or without paclitaxel plus filgrastim in advanced endometrial carcinoma: A Gynecologic Oncology Group Study.
J Clin Oncol 22(2004):2159-2166
3.) Miller D, et al.:
Randomized phase III noninferiority trial of first line chemotherapy for metastatic or recurrent endometrial carcinoma: A Gynecologic Oncology Group study.
Gynecol Oncol 125(2012):771-773
4.) Thigpen JT, et al.:
A randomized comparison of doxorubicin alone versus doxorubicin plus cyclophosphamide in the management of advanced or recurrent endometrial carcinoma: A Gynecologic Oncology Group study.
J Clin Oncol 12(1994):1404-1414
5.) Thigpen JT, et al.:
Phase III trial of doxorubicin with or without cisplatin in advanced endometrial carcinoma: A Gynecologic Oncology Group study.
J Clin Oncol 22(2004):3902-3904
6.) Gallion HH, et al.:
Randomized phase III trial of standard timed doxorubicin plus cisplatin versus circadian timed doxorubicin plus cisplatin in stage III and IV or recurrent endometrial carcinoma: A Gynecologic Oncology Group Study.
J Clin Oncol 21(2003):3404-3413
7.) Fleming GF, et al.:
Phase III randomized trial of doxorubicin + cisplatin versus doxorubicin + 24-h paclitaxel + filgrastim in endometrial carcinoma: A Gynecologic Oncology Group study.
Ann Oncol 15(2004):1173-1174
8.) Meyer L, et al.:
Postoperative Radiation Therapy for Endometrial Cancer: American Society of Clinical Oncology Clinical Practice Guideline Endorsement of the American Society for Radiation Oncology Evidence-Based Guideline.
JCO 2015;33:2908-2913. DOI 10.1200/JCO.2015.62.5459
9.) Liu J F, et al.:
Phase II Study of the WEE1 Inhibitor Adavosertib in Recurrent Uterine Serous Carcinoma.
J Clin Oncol 2021;39:1531-1539
10.) Kong A, Johnson N, Kitchener HC, et al.:
Adjuvant radiotherapy for stage I endometrial cancer.
Cochrane Database Syst Rev. 2012;4:CD003916
11.) Kong A, Johnson N, Cornes P, et al.:
Adjuvant radiotherapy for stage I endometrial cancer.
Cochrane Database Syst Rev. 2007;2:CD003916
12.) Kong A, Johnson N, Kitchener HC, et al.:
Adjuvant radiotherapy for stage I endometrial cancer: An updated Cochrane systematic review and meta-analysis.
J Natl Cancer Inst. 2012;104:1625–1634
13.) Hind D, Wyld L, Beverley CB, et al.:
Surgery versus primary endocrine therapy for operable primary breast cancer in elderly women (70 years plus).
Cochrane Database Syst Rev. 2006;1:CD004272
14.) Eskander RN, Sill MW, Beffa L, et al.:
Pembrolizumab plus Chemotherapy in Advanced Endometrial Cancer.
New England Journal of Medicine 2023;388:23 2159-2170
doi: 10.1056/NEJMoa2302312
15.) Fader AN, Roque DM, Siegel E, et al.:
Randomized Phase II Trial of Carboplatin-Paclitaxel Versus Carboplatin-Paclitaxel-Trastuzumab in Uterine Serous Carcinomas That Overexpress Human Epidermal Growth Factor Receptor 2/neu.
Journal of Clinical Oncology 2018;36(20):2044-2051
doi: 10.1200/JCO.2017.76.5966
16.) Kommoss F K, et al.:
L1CAM further stratifies endometrial carcinoma patients with no specific molecular risk profile.
British Journal of Cancer 2018:119(4)480–486
doi: 10.1038/s41416-018-0187-6
